The headline refers to a tragic situation involving Adriana Smith, a 30-year-old pregnant woman from Atlanta, Georgia, who was declared brain dead after suffering from severe headaches and blood clots in her brain.
Here’s a breakdown of the situation:
- Medical Emergency: In early February 2025, Smith, who was nine weeks pregnant, experienced intense headaches. Her mother, April Newkirk, stated that the hospital initially didn’t take her symptoms seriously, and a CT scan wasn’t performed.
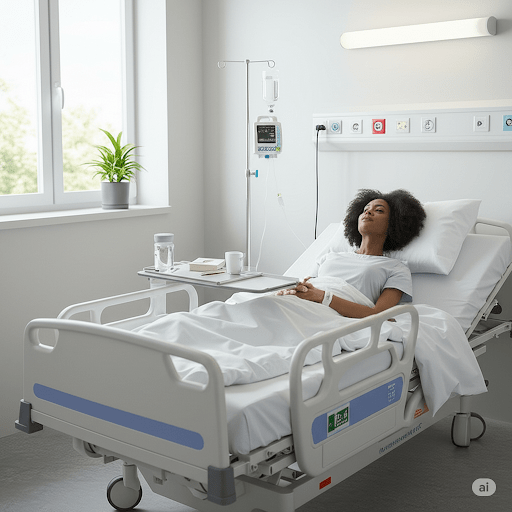
- Brain Death: Smith’s condition deteriorated, and she was eventually declared brain dead after suffering multiple blood clots in her brain.
- Georgia’s Abortion Law: Georgia’s Living Infants Fairness and Equality (LIFE) Act, also known as the “Heartbeat Bill,” bans abortions once a fetal heartbeat is detected, typically around six weeks.
- Legal Gray Area: While the law has exceptions for medical emergencies, Smith’s case fell into a legal gray area. Because she was brain dead, doctors reportedly argued that she was no longer considered at risk, and the law required them to maintain life support until the fetus reached viability (around 32 weeks).
- Family’s Anguish: Smith’s family, particularly her mother, April Newkirk, expressed immense distress over the situation. She described it as “torture” to see her daughter’s body being kept alive by machines when she was essentially gone. Newkirk felt that the decision of whether to continue life support should have been left to the family, regardless of whether they would have chosen to terminate the pregnancy.
- Concerns About the Fetus: The family also had concerns about the fetus’s health, as doctors reportedly found fluid on its brain and said it might not survive or have severe disabilities if it did.
- Ethical and Legal Debate: This case highlights the complex ethical and legal issues surrounding abortion bans and their implications in situations involving brain-dead pregnant women. It raises questions about bodily autonomy, the rights of the fetus, and the emotional toll on families in such heartbreaking circumstances.
If I were in any of the positions in this scenario, I’d be facing an agonizing situation with no easy answers. Here’s how I might approach it:
If I were Adriana Smith:
- Prior to the emergency: I would ensure I had a clear advance directive outlining my wishes regarding medical care in situations where I’m unable to make decisions. This would ideally address pregnancy and life support. I’d discuss this thoroughly with my family.
- During the initial medical situation: I would advocate strongly for my own health and well-being. If I felt my concerns weren’t being taken seriously, I’d insist on thorough testing, including a CT scan, and seek a second opinion if necessary.
If I were April Newkirk:
- In the immediate aftermath: I would be devastated and overwhelmed with grief. My priority would be to ensure my daughter’s comfort and dignity. I would fight fiercely for my daughter’s wishes, as expressed in any advance directive, or, in the absence of that, what I believed she would have wanted.
- Regarding the legal battle: I would seek legal counsel specializing in medical ethics, reproductive rights, and end-of-life care. I would explore all legal avenues to challenge the application of the law in this specific case, arguing for the recognition of my daughter’s brain death and the right to make decisions about her body.
- Supporting my family: I would seek emotional support for myself and my family, including grief counseling. I would try to be a source of strength for my grandson and help him understand the situation in an age-appropriate way.
If I were one of the physicians:
- Initial assessment: I would prioritize a thorough and timely medical evaluation of the patient, including appropriate diagnostic testing (in this case, a CT scan) to identify the cause of the symptoms.
- Upon declaration of brain death: I would consult with medical ethics experts, legal counsel, and other specialists (e.g., maternal-fetal medicine) to navigate the complex legal and ethical issues.
- Balancing legal obligations and patient/family wishes: I would advocate for a solution that respects the patient’s dignity and the family’s wishes, while also considering the legal framework. If the law created an untenable situation, I would explore all possible interpretations and legal challenges. I would document all decisions and rationales meticulously.
- Fetal considerations: I would provide the family with comprehensive information about the fetus’s condition, potential outcomes, and the risks and benefits of continuing the pregnancy.
Overall:
This case highlights the urgent need for:
- Clearer legal frameworks: Laws regarding abortion and end-of-life care need to be more nuanced and address the complexities of situations like this.
- Improved medical training: Healthcare professionals need better training in recognizing and responding to medical emergencies in pregnant patients, as well as in navigating ethical dilemmas.
- Emphasis on patient autonomy: Advance directives and patient wishes should be given greater weight in medical decision-making, even in complex situations.
- Compassionate care: Above all, the focus should be on providing compassionate and ethical care to both the patient and their family, minimizing suffering and respecting their dignity.

You must be logged in to post a comment.